Physicians in their residency are bearing the brunt of a healthcare system in crisis
You’ve just been in a life-threatening car accident. You are rushed to the emergency room and are cleared for immediate life-saving surgery. What if you knew that the doctor performing surgery on you could be working their 25th consecutive hour? Would you feel safe and that this medical professional would not commit any mistakes? Would you trust their judgement? Likely not.
Yet, this is often the reality of Ontario’s healthcare system. Ontario physicians in their residency face being underpaid, overworked, and consistently subjected to harsh workplace environments; being a resident is an intensely demanding task.
A physician’s residency is defined as a time when they “work under the supervision of experienced physicians and receive hands-on training in their chosen specialty,” per StandYou. Further adding to this workload, they must “attend academic and clinical teaching sessions and are expected to participate in research and scholarly activities.”
The Professional Association of Residents of Ontario (PARO), has rules in place to help prevent residents from being overworked yet, a medical resident who preferred to stay anonymous (we’ll call them Sherry) detailed how these rules are treated more like “guidelines” than actual regulations. There is no regulating body to enforce these rules and residents themselves are powerless to speak out against these rules.

Sherry recounted how they worked over the supposed limit of 26 hours straight an average of six times per month.
Due to the fact there is no external body keeping these regulations, the only people to complain to are the more senior-level doctors. Getting a job after residency is highly dependent on references and these same senior-level doctors are the ones writing said references. “If you complain,” said Sherry, “you wouldn’t expect to have a good reference from the person you complained to.”
Dr. Sonja Wakeling, president of PARO, detailed how PARO has multiple initiatives in place to help alleviate the strain being placed on residents. Things like Night Share models, Tuck-In rounds and Drive-Share Reimbursement programs are all initiatives that are designed to help ease the tremendous burden of fatigue being placed on residents.
For most faculties of medicine, the average period for residents is five years. Depending on what you specialize in, that time period can look like five years of little to no social life, five years of consistent lack of sleep and high stress levels and five years of “being treated as nothing more than a number” according to Sherry.
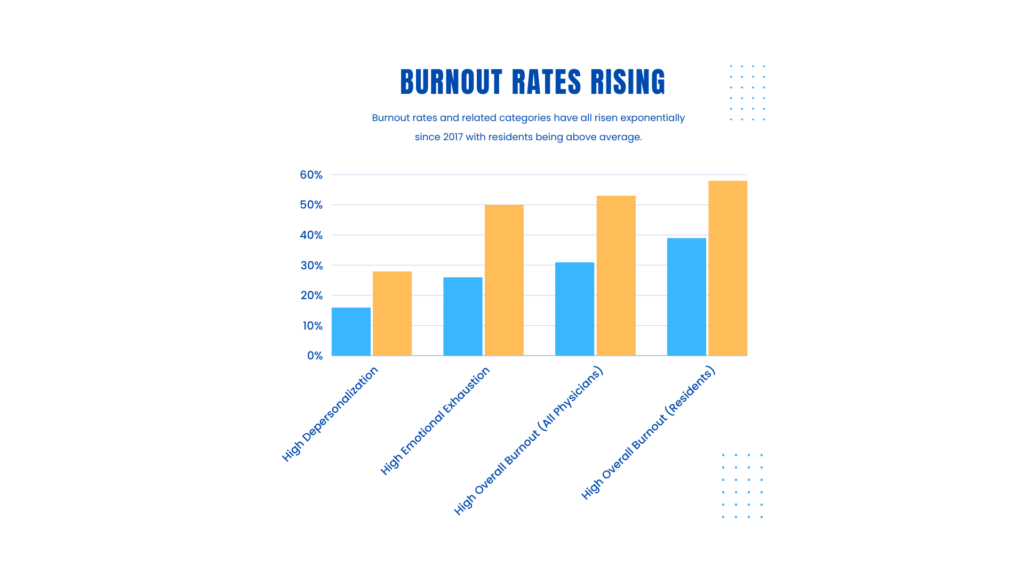
“Our healthcare system is in crisis,” says Dr. Kathleen Ross, President of the Canadian Medical Association (CMA). According to the National Physician Health Survey conducted by the CMA, the level of physicians who have experienced burnout has jumped by more than 20% between 2017 and 2021. And that number has likely risen since then, with medical care in greater need than ever.
Highlighting the fatigue aspect, Dr. Wakeling emphasized the importance of mitigating the risks of being tired, recognizing exhaustion and empowering residents to say they’re tired and need to rest.
A day in the life of a resident can look vastly different depending on the needs of patients. Work days can range from 12 hours to over 30 hours. It’s a regular occurrence to be called into work in the middle of the night, or after just getting home from work. This constant need creates a feeling of overwhelming dread as it’s very easy for physicians to fall behind on their research responsibilities, physical fitness as well as social lives. Their lives become consumed by their job and this isn’t healthy for anyone.
“The biggest challenges physicians face,” said Dr. Ross, “are the workload, the complexity and the lack of ability to access the resources that we need to manage the patients.”
As if working chronically long shifts wasn’t enough, it’s not uncommon for them to come home and research for hours. In fact, according to a survey by the Canadian Federation of Independent Business, Canadian doctors spend over 18 million hours a year on unnecessary administrative work. The workplace culture often treats speaking out and/or complaining about the system as open defiance that is punishable through indirect methods such as increased workloads, tougher assignments and more on-call time. This administrative burden can often take away not just a physician’s time to care for patients, but also their love for doing so.
Sherry said that they are responsible for at least six hours’ worth per week of administrative tasks like preparing hospital rounds, completing patient records at home and conducting research. They often feel behind and this stress can build up quickly.
This workload can seem overwhelming, and there isn’t much in place to take proper care of physicians who feel the effects of such a broken system.
According to Sherry, there are resources in place to help ensure a healthy work-life balance yet, residents often don’t have the time to use the resources provided.
“Our insurance does provide coverage for us but it’s very hard to get time off. I mean, we work Monday through Friday from 6 a.m. to 6 p.m. We don’t really have an off day. Most of these other professionals, who work with mental health for example, are only available Monday to Friday. So what time is there for us to go see them?”
Dr. Wakeling emphasized that it’s a complex issue that involves more than just residents. Fatigue is different for everyone and different residents face different challenges depending on their location and specialty. “It’s very team-based,” said Dr. Wakeling, “and we need to find ways to build structures that don’t rely on residents.”
Yet, the reality is that for a large number of residents, the initiatives aren’t enough. They’re sucked into a culture of putting your head down and not complaining, no matter what and this is certainly taking its toll. As the demand for healthcare grows in both scale and complexity, residents are suffering the brunt of it.
